Interstellar travel is a lifelong dream of humanity and there is no doubt that the duration and frequency of human spaceflights will increase in the future. However, the exposure to weightlessness and confined spaces sharply reduces the functional load on the human skeleton and affects bone health. Here, the authors discuss their research in this area.
The human skeleton has evolved under the conditions of the Earth’s gravitational field, along with the physiological mechanisms of bone tissue remodelling which include maturing and resorption. The balance of these constantly occurring processes determines the properties of the bone formed under new conditions. As a result, the decrease in functional loads during a space mission poses a potential danger to the skeleton, and in consequence to the health of the crewmembers.
 Valery Novikov with cosmonaut Anna Kikina as she undergoes osteodensitometry examination as part of her participation in the SIRIUS-17 experiment.
Valery Novikov with cosmonaut Anna Kikina as she undergoes osteodensitometry examination as part of her participation in the SIRIUS-17 experiment.
Research techniques
The decrease in functional loads during a space mission poses a potential danger to the skeleton
This area of research involves monitoring, data accumulation, physiological assessment of health risk, and the potential to predict problems and prevention.
The techniques for examining bone tissue condition include a wide range of clinical diagnostic manipulations: nutrition and physical activity monitoring, anthropometric characteristic evaluation, tracking of body weight and composition, research into bone microarchitecture using quantitative computed tomography, bone marker content analysis and mineral metabolism and analysis of the acid-base state and blood gases, and the analysis of a number of immune system parameters.
However, measuring bone mineral density (BMD) with dual-energy X-ray absorptiometry is the basic method for assessing the well-being of the skeleton. BMD measurement of skeleton elements is convenient for case monitoring, namely in the lumbar vertebrae and the proximal epiphysis of the femur (including the femoral neck), and is regarded as the World Health Organization (WHO) gold standard. These skeletal elements are important as they comprise about 70 percent of the total mass of metabolically active spongy bone in the entire skeleton.
Any measure of change assumes, as a basis for comparison, the maximum values observed, which are intrinsic to young people, and is expressed as a standard deviation (SD). Values that deviate by less than 1 SD are within normal limits; values between -1 SD and -2.5 SD are classified as osteopenia (reduced bone density); and values less than -2.5 SD are classified as osteoporosis (severe osteopenia). The WHO experts have formulated these criteria on the basis of epidemiological data analysis of women during menopause. The record shows that postmenopausal women ‘physiologically’ lose BMD in the lumbar vertebrae by up to two percent per year, while more than a third of them suffer osteoporosis. In men, the negative change across the years is minimal.
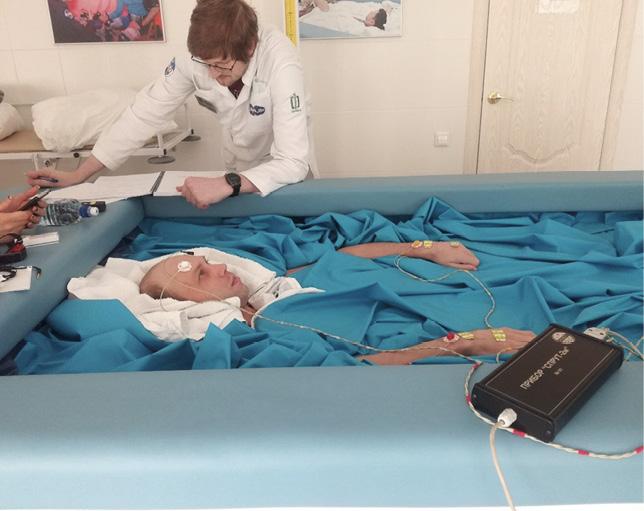
 Blood collection to assess hormonal state and analyse bone tissue biochemical markers of test subjects under dry immersion conditions.
Blood collection to assess hormonal state and analyse bone tissue biochemical markers of test subjects under dry immersion conditions.
Experiment results
Is it possible to provide long-lasting support for the skeleton during and after spaceflight and avoid excessive risks to human health?
To gain a better understanding of the effect of the limited amount of space in spacecraft on the skeleton, experts monitored changes in ground-based isolation experiments in a pressurised facility lasting from seven to 520 days. For good measure, the experimental subjects underwent head-down bed-rest testing (with a head of bed inclination of 5-8 degrees for experiment durations from seven to 120 days) and ‘dry immersion’ (from three to 21 days) to estimate the microgravity effect on bone tissue and the associated redistribution of fluids in the upper body.
Our observations as part of isolation experiments involving mixed crews – namely, the MARS-500 and SIRIUS international projects - showed high variability in BMD findings, both in the lumbar vertebrae (from -7.39 to +2.6 percent) and in femoral neck (from -6.1 to +2.82 percent).
Actual cosmonauts undergo densitometric examinations at the stage of space training and immediately on completing a mission. Clearly, osteoporosis is unacceptable for the cosmonaut profession; in the case of detecting osteopenia, physicians apply an individual approach, using the specified acceptable values of BMD according to the international health standard for the International Space Station (ISS).
Along this line, at the end of a six-month spaceflight, one may commonly characterise BMD as the ‘norm’, even given that the losses are several times greater than the annual ‘physiological’ ones registered in humans. They average 5.4 percent in the lumbar vertebrae and 8.5 percent in the femoral neck.
Such a high rate of BMD decrease practically never occurs on the ground, and the nature and localisation of changes in spaceflight conditions also differ from those in terrestrial conditions. More than once, we have observed cases of uneven and even oppositely directed BMD changes in the areas checked, while the femoral neck always demonstrates losses in mineral density.
 Analysing body composition behaviour and body fluids under ‘dry’ immersion conditions (Sprut-2 Bioimpedance Analyzer, Russia).
Analysing body composition behaviour and body fluids under ‘dry’ immersion conditions (Sprut-2 Bioimpedance Analyzer, Russia).
Numerous densitometric examinations of cosmonauts keep track of the individual specificity of both the skeleton’s initial state and its response to the exposure to spaceflight factors. For example, cosmonauts with high BMD often experience lower losses in flight, so one may apply this feature in predicting bone tissue change in such subjects.
However, we have not yet defined a true-to-fact connection between the initially low BMD and its loss value in microgravity, so it is currently impossible to calculate whether the skeleton of anyone having low BMD will approach a critical level of demineralisation during a long-term (1.5 to two year) space mission. Restoring BMD after missions lasting about six months requires between one and three years.
Besides measuring BMD in standard body areas with set normal values, expressed in grams per projected area (g/cm2), dual-energy X-ray absorptiometry makes it possible to measure bone mineral content (BMC) in body areas such as the head, arms, ribs, pelvis and legs in grams. BMC is not applicable or intended for diagnosing osteoporosis, but it is applicable for case monitoring for scientific research purposes.
The astronauts’ BMC loss is greater in the skeleton areas bearing large gravitational loads, primarily in the skeleton’s lower torso (lumbar vertebrae, pelvic bones and femur). At the same time, the BMC in the bones of the upper torso has a clear tendency to increase, which, according to some researchers, may be a consequence of the redistribution of body fluids in the head. The BMC may decrease further in the early return to Earth, as the adaptive bone remodelling mechanism responds to the ‘returning’ mechanical load on the skeleton.
Space missions lasting one year or more are of particular interest for planning interplanetary missions and human activities on other space objects. BMD losses after such missions do not exceed those at ‘half mission time’. However, the small number of observations, combined with the high individual variability of the results obtained, does not allow us to draw reasonable conclusions.
 CT scanning of lower leg bones of tester Alexey Fedorov (above) during SIRIUS-21, using the XCT2000L peripheral X-ray computer tomograph (pQCT) (DLR)and (above left) studying changes in body composition and body fluids in the frame of the Eskiz (Sketch) isolation experiment using Sprut-2 bioimpedance analyzer, Russia.
CT scanning of lower leg bones of tester Alexey Fedorov (above) during SIRIUS-21, using the XCT2000L peripheral X-ray computer tomograph (pQCT) (DLR)and (above left) studying changes in body composition and body fluids in the frame of the Eskiz (Sketch) isolation experiment using Sprut-2 bioimpedance analyzer, Russia.
Open questions
There are no definite conclusions regarding the behaviour of women’s bones in spaceflight conditions and more research into gender differences in the context of skeleton response to the extreme conditions is required
We have assumed that the physiological mechanisms enabling changes in the skeleton in microgravity become active at the tissue, cellular and molecular level: this includes osteocitic osteolysis, collagen-crystal uncoupling, slowing down of osteoblastic histogenesis, reducing calcium intestinal absorption and kidney reabsorption, and osteoclastic resorption activation.
One might perceive the observed phenomena as ‘aggressive but reversible osteopenia’, that is, as an effect of the skeleton’s adaptation to the changing mechanical load. However, a number of issues that constitute foreseen hazards to astronaut health are as follows:
- Similar to clinical experience, we assess BMD in the areas with predominant trabecular (highly porous) bone tissue - the lumbar vertebrae and proximal femoral epiphysis - since we find that these areas respond more amenably to external stimuli. Meanwhile, our observations often show major losses in other skeleton areas rich in cortical (compact) bone tissue, such as the pelvic bones and lower limb. The question is, to what extent does the densitometry reflect a person’s bone status in standard areas under extreme conditions?
- The MPC, especially with high initial values, may formally remain within the “normal” levels but suffer significant losses (more than six percent over six months). Such a high rate of decrease in BMD does not occur on the ground. Is it an option to accept such bone behaviour as safe?
- The lack of onboard monitoring of bone state dynamics does not allow us to discuss the equable BMD loss and stabilisation over a certain period. Is it fair to assume that BMD becomes stable at a level adequate to the functional load and will this level be safe for terrestrial and planetary activities?
- Measuring BMD does not produce a quality image of bone tissue as a structure and the specificity of bone architectonics evaluation in microgravity requires further study. What are the strength characteristics of an off-Earth matured bone?
- There are very few studies on bone dynamics in women under spaceflight conditions and more research into gender differences in the context of skeleton response to the extreme conditions is required. To what extent are they mission-critical?
All of the above makes it impossible to answer the vital question: is it possible to provide long-lasting support for the skeleton during spaceflight and avoid excessive risks to human health?
The relatively small number of observations hampers the physiological assessment and prediction of changes in the skeleton under spaceflight conditions. However, successfully completed long-term space missions inspire optimism and offer no justification to the view that risks to the skeleton will be excessive – at least for the present spaceflight durations and in view of currently existing preventive measures. Despite this, longer missions and distances from Earth, coupled with the number of crewmembers, will require detailed answers to the questions posed above.
 Figure 4. Elena Luchitskaya, a participant in the SIRIUS-17 experiment, undergoes computed tomography of lower-leg bones.
Figure 4. Elena Luchitskaya, a participant in the SIRIUS-17 experiment, undergoes computed tomography of lower-leg bones.
About the authors
Valery E Novikov is Leading Researcher of Bone & Metabolic Effects of Microgravity Research Laboratory at the Institute of Biomedical Problems of the Russian Academy of Sciences (IBMP RAS). He has a PhD in Medicine.
Anna R Kussmaul is Senior Researcher, Deputy Head of Department at the IBMP RAS. She has a PhD in Biology and is a Full Member of the International Academy of Astronautics.
Galina Yu Vassilieva is a Head of Bone & Metabolic Effects of Microgravity Research Laboratory at the IBMP RAS and a Head of Planning Research & Staff Procedures of the SIRIUS project. She has a PhD in Medicine and is a Full Member of the International Academy of Astronautics.














